
What is Pars Interarticularis Defect? Symptoms, Treatment, & Causes
Tuesday, June 8, 2021
We all know that feeling of an aching lower back. How can you know if that pain is a simple soreness or the result of a stress fracture, or maybe even a pars defect?
Pars defect, otherwise known as spondylolysis is a fracture within the pars interarticularis of the vertebral arch in the spinal column. To put it simply, the defect is a stress fracture of the bones of the lower spine that results in lower back pain. Rather than being in the center of the back, this back pain is usually on one side of the back. When a pars defect does not heal it can lead to spondylolysis which is a permanent pars fracture on both sides of the spine.
When this occurs, the spine can slip backwards over time which would result in a more serious condition of what is commonly referred to as spondylolisthesis. This, then increases the possibility of a degenerative vertebra and further back conditions in adulthood. The good news that these back problems can be prevented with early diagnosis and treatment methods.
It may not sound too serious but like other fractures, a stress fracture is a break in the bone. It's only referred to a “stress” fracture because it develops as a result of repetitive stress and overuse that is usually associated with sports and activity. This differs from a specific acute event or injury which may create pain suddenly and quickly from a specific event or injury.
See below an illustration of the spinal column and the location of a Pars Fracture
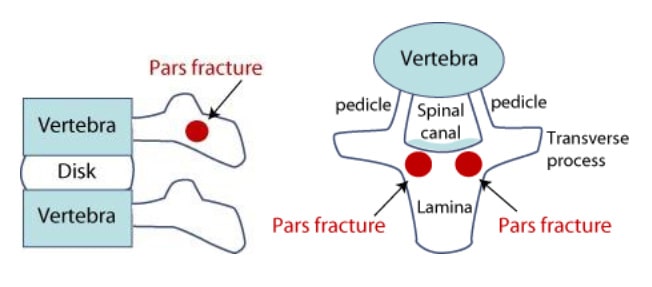
Image Reference: https://www.hss.edu/condition-list_Spondylolysis-Spondylolisthesis.asp
How do you know if you or your child suffer from a pars defect?
The pars defect is one of the most common causes of lower back pain in younger athletes. The lifetime prevalence of lower back pain with a pars defect in those aged 11-17 years has been reported to be as high as 30.4% among adolescents participating in sports. The condition is more common in males; 2-1
The structure of a pars bone is small, and it grows longer during adolescent growth. Therefore, it is very thin and weak, and very much prone to injury during young adolescence. Kids and teens who play sports and do activities that can strain the lower back or that involve a lot of lower-back stretching — like football, weightlifting, wrestling, cricket – bowling action, gymnastics, volleyball, ballet, and golf — are especially likely to have these problems.
Placing extra strain on this area of the spine during childhood increases the chance that a pars defect will occur.
Symptoms of a pars defect usually have one of the following;
- pain in the lower centre back that might feel like a muscle strain
- pain in the thighs and buttocks
- stiff muscles and tenderness in the lower back region
- muscle tightness, especially in the hamstring muscles
- Pain radiating down one or both legs
- Numbness, tingling, and weakness in legs
Diagnosis of Pars Stress Fracture
Since a pars fracture is a break in the bone, only rest and time will promote healing. Most people with a pars defect do not require surgery with anti-inflammatory medications, Physiotherapy and recovery the recommended means of dealing with a pars stress fracture.
Typically, the average recovery rate of Pars Fracture can be anything from between 6-12 weeks.
Recovery is the most important aspect for the initial stages of a pars stress fracture. With the guidance and implementation of Physiotherapy, individuals with a stress fracture should expect a series of strengthening exercises for the abdominal and low back muscles to combat the pain and rehabilitation from their Physiotherapist.
In some cases, a complete recovery from a pars stress fracture can take as long as 6 months.
When symptoms and pain are not relieved with nonsurgical treatments patients may require surgery. Surgical options for a pars defect include a pars repair versus a lumbar fusion.
Injections are another alternative but more commonly used for in the adult population. Injections might help control the pain enough to least keep you functional. In some cases, injections will have very little affect for some adults and if they do work, the injections do have the tendency to wear off. However, the positive implications of using injections is that they are a very low risk and less invasive technique to adopt.
How can you prevent the possibility of this fracture and pain in your spine?
There are actually a few things that you can do to avoid getting a pars stress fracture including;
- Taking a break from sports every few days
- Maintaining good physical condition during the off season
- Increasing high impact activities gradually
- Increasing hours in sports gradually
- Avoiding year-round participation in sports
- Maintaining flexibility in the hamstrings and hip flexors
- Increasing strength in the lumbar and core muscles.
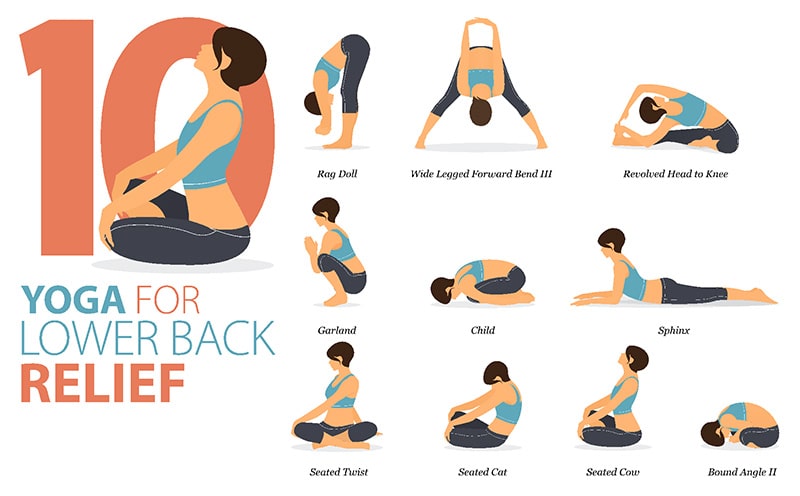
- Yoga movements and exercises.
How is pars defect treated?
In most cases, pars defect is treated with medication, muscle relaxers and rest. However, sometimes surgery will be required. Your Physiotherapist may also prescribe a lumbar back brace in the acute stages of pars defect that will aid in the treatment process.
Is a pars fracture serious?
It depends. Like any fracture, a pars defect is relatively serious and will require some form of treatment. However, it can be difficult to detect and makes things a bit trickier than when you break an arm or foot.
Since pars defect is common among children who are quite active or participate in a sport of some kind, the healing rate for bones is rather quick meaning that most children recover with not much more than a bit of downtime.
However, on some occasions, the symptoms of a pars defect won't show up until later in life. Overall, yes, a pars fracture is serious but not life-threatening and can be treated.
How long does a pars defect take to heal?
A pars defect takes about six to 12 weeks to heal but it could take up to six months to see a full recovery. However, the rate at which you recover from a pars defect depends on variables such as:
- Your current health
- How you've managed your recovery (ie. working with a physiotherapist, taking enough time off from physical activity)
- The severity of your pars defect
As with anything, there's no one size fits all recovery time. It's important to speak with your doctor and physiotherapist about how long recovery should take for your particular situation.
How do you sleep with a pars defect?
The best position to sleep with a pars defect is in a reclined position as if you were sitting in a recliner chair.
If you have a recliner, you might even try sleeping in the chair for a few nights to see if it helps relieve the back pain from your pars defect. If not, you might use a stack of pillows to prop yourself up in bed. You might also place a pillow under your knees to further the relief.
There are also adjustable beds where you can change your side to mimic the shape of a recliner whilst still sleeping next to your partner. So, if you find that it relieves your back pain to some extent, you might consider investing in one of these adjustable beds.
Keep in mind that these are only general guidelines and everyone's body is different, therefore requiring different sleeping positions. Try out a few different options of pillows propping you up or placed underneath your knees to find your ultimate sleep spot.
How common is pars defect?
Pars defect is relatively common, affecting one out of every 20 people. The most common cause is repetitive stress on the lumbar vertebrae.
A pars defect is also more common in children since children tend to be more physically active than adults. However, you might not start experiencing the signs of a pars defect until you're older, even if it actually occurred in childhood.
If you are experiencing back or leg pain, and think you may have a pars defect, Physio Inq can help!
We have a team of Physiotherapists In-Home Physiotherapists and Exercise Physiologists all across Australia that can assess you and advise you on the best course of action to take.. Contact us by phone at 1300 731 733 or find a location nearest to you to get started!
This article was originally written by Jonathan Moody from Physio Inq

